Depression, according to WHO, is currently one of the most common and life-threatening mental diseases. It is estimated that as many as 350 million people worldwide suffer from it. In turn, insomnia affects up to 30% of the population or every third person on Earth! As it turns out, both depression and insomnia have a lot in common. Why?
The common denominator
Depression, although we often use this word to describe a bad mood, is a group of complex chronic conditions such as the blues, emptiness, loss of energy, sadness, irritability, and lack of concentration. A person that struggles with this disease gradually loses joy in life and self-confidence and feels unjustified fear or guilt. In addition to the above symptoms, insomnia characterises an early symptom. Sleep disturbances affecting depression are not limited to just problems falling asleep. People suffering from it often sleep many hours during the day yet continue to feel tired and lethargic.
This fact means that, while depression almost always causes sleep problems, it may also be true that chronic sleep disorders can cause a mental disorder of a depressive nature! After all, sleep has a tremendous impact on our health and the functioning of the entire body. Persistent fatigue disrupts the brain, endocrine, and nervous systems and impairs many of the processes they regulate. As a result, we feel the physical effects of sleep deprivation, such as fatigue and lack of energy, and the mental effects – frustration, sadness, depression, unwillingness to interact with other people, or the inability to focus.
A recipe for body and soul
Both depression and insomnia are called “a disease of the soul and body,” and they are even confused with each other. And no wonder, because they have similar symptoms and root causes, which is difficult to clearly and quickly classify. However, this does not mean that if we suspect one of them, we should not try to treat it – quite the contrary! Consulting with a specialist (in this case, a psychiatrist or psychotherapist) will give us a chance for an accurate diagnosis and effective treatment. If, in addition to depression, we are also diagnosed with insomnia, it is important to treat both disorders simultaneously. It is extremely important to recognise the defective patterns of thinking and behaviour that led to the emergence and perpetuation of insomnia and then replace each of them individually by developing habits that will regulate sleep physiology.
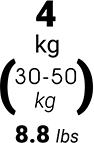
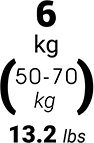
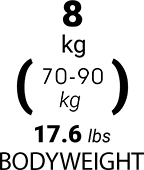
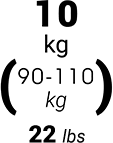
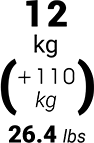
In addition to using a variety of techniques, such as activity and rest schedules, relaxation exercises, or keeping a dream diary, patients can also use a weighted (or sensory) blanket, which has positive effects in supporting the treatment of both depression and insomnia. Using weight on the body as a therapeutic method has been used for over 30 years, and weighted blankets or duvets are the most popular supporting tools. How do they work? Skin receptors stimulated by pressure send positive impulses and information about a specific position of the body in a given place and space to the brain. These impulses, in turn, determine subsequent hormonal processes, as the brain interprets our position as unchallenged, “covered” as in the parent’s arms. The effect? The brain decreases the production of cortisol (the stress hormone) and increases the level of serotonin (the happiness hormone).
If you suspect that depression or insomnia affects you, be sure to go to a specialist, and you will increase your chances of a speedy recovery.